For many of my grownup life, I’ve felt helpless about being obese. Once I met with a health care provider a couple of years in the past to debate my excessive ldl cholesterol, he held up a hunk of fake flesh meant to mannequin a pound of extra fats and inspired me to lose 20 of stated gelatinous blobs. Maybe, he recommended, I ought to eat much less pink meat and begin exercising. I nonetheless keep in mind his perplexed stare after I advised him I had a longtime gymnasium routine and had been a vegetarian for the higher a part of a decade.
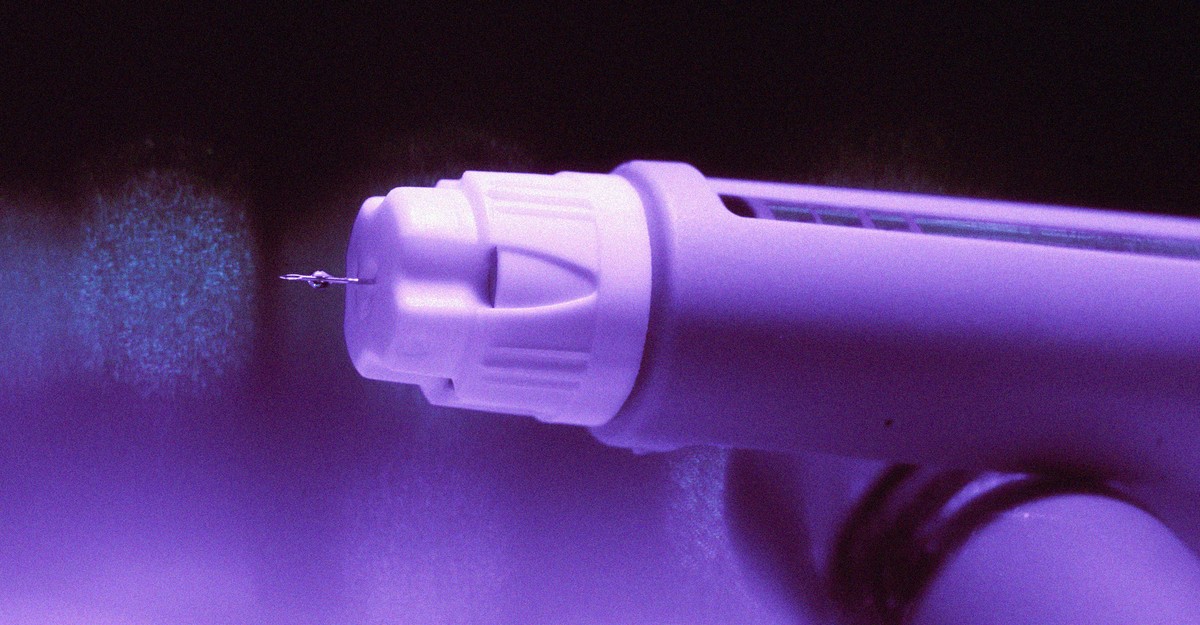
Beginning an weight problems drug was imagined to be successful. The times of being winded after strolling up the steps to my condominium, and shopping for T-shirts marketed for guys with massive bellies, would lastly be over. Or so I believed. My medical health insurance didn’t cowl Wegovy or Zepbound, the 2 GLP-1 medication permitted for weight reduction. (Each drugs are additionally bought for diabetes, beneath the model names Ozempic and Mounjaro, respectively.) Regardless of my pleading, the insurance coverage firm wouldn’t budge.
For all of the hype over GLP-1s, Individuals have struggled to entry these weekly injections. Seniors can’t get these medication as a result of Medicare is barred by regulation from masking them for weight problems. Drugmakers beforehand couldn’t make sufficient of the medication to maintain up with demand, prompting the FDA to formally declare a scarcity. The provision points have now abated, however getting these medication has in some way grow to be even tougher. The issue is that insurance coverage firms are refusing to cowl them.
Contemplate Zepbound, the simpler GLP-1 for weight reduction. Greater than half of all personal insurance policy don’t cowl Zepbound in any respect, up from 18 p.c final 12 months. That’s based on current knowledge from GoodRx, a web site that compares prescription-drug costs. Plans usually tend to cowl Wegovy, based on GoodRx, however a dwindling share allow you to get the drug with out first going by obstacles that will find yourself curbing entry.
Eli Lilly, the pharmaceutical firm that makes Zepbound, blames the dearth of protection on the stigma of weight problems. “Regardless of weight problems being acknowledged as a power, complicated illness, insurance coverage and federal packages nonetheless don’t present broad protection to individuals who stay with this illness,” the corporate wrote in a press release. However that isn’t the total story. Many Individuals get medical health insurance by their job, and GLP-1s are so costly that many firms merely can’t afford the medication. It’d really feel like magic when insurance coverage picks up the tab in your prescriptions, however a part of these value financial savings are literally paid by your employer. A month’s provide of a GLP-1 retails for at the very least $1,000. When you think about that roughly three-quarters of American adults are obese or overweight, employers could possibly be confronted with a whole lot and even 1000’s of GLP-1 payments every month. (Individuals who’re obese however not overweight are eligible for GLP-1s if they’ve excessive ldl cholesterol or sure different well being circumstances.) “It’s brutal, and it’s forcing employers to make powerful choices,” James Gelfand, the president of the ERISA Business Committee, a lobbying group that advises giant employers on health-insurance points, advised me.
[Read: Ozempic or bust]
For firms seeking to handle the prices, “the answer to the issue is simply making it tougher to get the medication,” Ameet Sarpatwari, a drug-pricing skilled at Harvard, advised me. Smaller firms are particularly struggling; a survey launched final week by the Kaiser Household Basis discovered that simply 16 p.c of employers with 200 to 999 workers are masking Wegovy or Zepbound, in contrast with 43 p.c of employers which have 5,000 or extra workers. However even main firms are making sufferers undergo hurdles earlier than they will entry these medication. One of the crucial frequent insurance policies requires medical doctors to submit extra paperwork explaining why a affected person wants these medication earlier than a prescription might be picked up. That may not sound all that onerous, however peer-reviewed analysis reveals it delays sufferers from getting the medication their medical doctors say they want. In my expertise, it additionally requires sustained effort from the affected person to corral a health care provider’s workplace into submitting the required paperwork.
If employers have to put restrictions on the GLP-1s sufferers can entry, it will appear logical that they might begin with Wegovy. Notably, the drug prices about $300 extra a month than Zepbound—and it additionally works much less properly. (A head-to-head trial of the 2 drugs, funded by Eli Lilly, discovered that sufferers on Zepbound misplaced a median of 20 p.c of their weight, versus about 14 p.c for these on Wegovy.) However, it’s a lot tougher to get Zepbound than Wegovy. “You’ll be able to’t assume that simply being the most effective product signifies that you’ll be on the formulary,” Gelfand stated.
Insurers are basing their protection choices, partly, on “rebates,” reductions which are provided by drugmakers as a negotiating chip to steer insurers to cowl one product over a competitor. For instance, in July, CVS Caremark, a pharmacy-benefit supervisor employed by insurance coverage firms to assist decide which medication to cowl, started recommending Wegovy over Zepbound usually. Ed DeVaney, the president of CVS Caremark, advised me that the choice was made as a result of his firm deemed the 2 medication very comparable when it comes to efficacy, and since the deal represented “the best worth” for the well being plans and employers the corporate works for. However the transfer hasn’t been well-liked. Medical doctors favor Zepbound over Wegovy, based on prescribing knowledge analyzed by the analytics agency Truveta. Prescriptions might go unfilled as soon as sufferers understand that their insurance coverage firms received’t foot the invoice. (CVS Caremark is dealing with a class-action lawsuit filed by prospects who have been prescribed Zepbound however weren’t in a position to get it by their insurance coverage. )
With out insurance coverage protection, sufferers have to show elsewhere for these medication. Eli Lilly and Novo Nordisk promote their medication to sufferers straight for a serious low cost, however they nonetheless are prohibitively costly: A vial of Zepbound prices $500 a month when bought straight from the producer. Sufferers can go for cheaper variations of those medication which are made by compounding pharmacies, however they are often unreliable and unsafe. Neither of those alternate options have been options for me, they usually seemingly received’t be for a lot of Individuals. Though I attempted a couple of months of compounded medication, the dangers of injecting myself with a serum that hadn’t been reviewed for security by the FDA began to weigh on me. In the end, I used to be in a position to get on my fiancée’s insurance coverage, and now I lastly have entry to Wegovy. (Her plan refuses to cowl Zepbound.) However only a few sufferers can flip to this form of backup plan when their very own insurance coverage comes up brief.
GLP-1s are hardly excellent. They arrive with typically extreme negative effects, together with nausea, and the weight-loss outcomes final solely so long as individuals preserve taking them. However the upside for individuals with weight problems is simple. Finally, tens of millions of Individuals who’re ready for these medication ought to be capable to get them. Extra competitors ought to result in modestly bigger rebates, making it cheaper for employers to cowl these medication, Sarpatwari stated. Novo Nordisk is growing a brand new weight problems drug that scientific trials recommend rivals Zepbound in effectiveness, and Eli Lilly is testing a drug that might find yourself being much more efficient than the present merchandise in the marketplace. A number of firms, together with Novo Nordisk and Eli Lilly, are additionally growing oral variations of those medication for many who don’t need to inject themselves weekly. The brand new medication will nearly actually be dearer than these already in the marketplace, however they need to make it barely simpler for sufferers to entry older GLP-1 medication.
That future stays far-off. The beginning of the GLP-1 period targeted on the thrilling transformations sufferers have made on these medication. If one thing doesn’t change, the subsequent few years are going to concentrate on all of the individuals who may benefit from GLP-1s however are unable to entry them.