The euthanasia convention was held at a Sheraton. Some 300 Canadian professionals, most of them clinicians, had arrived for the annual occasion. There have been lunch buffets and complimentary tote baggage; attendees might look ahead to a Friday-night social outing, with a DJ, at an occasion house above Par-Tee Putt in downtown Vancouver. “Crucial factor,” one physician advised me, “is the networking.”
Which is to say that it might need been some other conference in Canada. Over the previous decade, practitioners of euthanasia have develop into as acquainted as orthodontists or plastic surgeons are with the mundane rituals of lanyards and drink tickets and It’s been so lengthy s exterior the ballroom of a four-star lodge. The distinction is that, 10 years in the past, what most of the attendees right here do for work would have been thought of murder.
When Canada’s Parliament in 2016 legalized the follow of euthanasia—Medical Help in Dying, or MAID, because it’s formally known as—it launched an open-ended medical experiment. In the future, administering a deadly injection to a affected person was towards the regulation; the following, it was as reliable as a tonsillectomy, however usually with much less of a wait. MAID now accounts for about one in 20 deaths in Canada—greater than Alzheimer’s and diabetes mixed—surpassing nations the place assisted dying has been authorized for much longer.
It’s too quickly to name euthanasia a way of life choice in Canada, however from the outset it has proved a case research in momentum. MAID started as a follow restricted to gravely unwell sufferers who had been already on the finish of life. The regulation was then expanded to incorporate individuals who had been affected by severe medical circumstances however not going through imminent loss of life. In two years, MAID might be made out there to these struggling solely from psychological sickness. Parliament has additionally really helpful granting entry to minors.
On the heart of the world’s fastest-growing euthanasia regime is the idea of affected person autonomy. Honoring a affected person’s needs is after all a core worth in medication. However right here it has develop into paramount, permitting Canada’s MAID advocates to push for growth in phrases that brook no argument, refracted by means of the language of equality, entry, and compassion. As Canada contends with ever-evolving claims on the appropriate to die, the demand for euthanasia has begun to outstrip the capability of clinicians to supply it.
There have been unintended penalties: Some Canadians who can not afford to handle their sickness have sought docs to finish their life. In sure conditions, clinicians have confronted unattainable moral dilemmas. On the identical time, medical professionals who determined early on to reorient their profession towards assisted loss of life not really feel compelled to tiptoe across the full, energetic extent of their devotion to MAID. Some clinicians in Canada have euthanized a whole lot of sufferers.
The 2-day convention in Vancouver was sponsored by knowledgeable group known as the Canadian Affiliation of MAiD Assessors and Suppliers. Stefanie Inexperienced, a doctor on Vancouver Island and one of many group’s founders, advised me how her a long time as a maternity physician had helped equip her for this new chapter in her profession. In each fields, she defined, she was guiding a affected person by means of an “primarily pure occasion”—the emotional and medical choreography “of a very powerful days of their life.” She continued the analogy: “I believed, Effectively, one is like delivering life into the world, and the opposite appears like transitioning and delivering life out.” And so Inexperienced doesn’t discuss with her MAID deaths solely as “provisions”—the time period for euthanasia that almost all clinicians have adopted. She additionally calls them “deliveries.”
Gord Gubitz, a neurologist from Nova Scotia, advised me that individuals usually ask him concerning the “stress” and “trauma” and “strife” of his work as a MAID supplier. Isn’t it so emotionally draining? In truth, for him it’s simply the alternative. He finds euthanasia to be “energizing”—the “most significant work” of his profession. “It’s a contented unhappy, proper?” he defined. “It’s actually unhappy that you simply had been in a lot ache. It’s unhappy that your loved ones is racked with grief. However we’re so glad you bought what you needed.”
Has Canada itself gotten what it needed? 9 years after the legalization of assisted loss of life, Canada’s leaders appear to treat MAID from a wierd, virtually anthropological take away: as if the way forward for euthanasia isn’t any extra inside their management than the legal guidelines of physics; as if continued growth is just not a actuality the federal government is selecting a lot as conceding. That is the story of an ideology in movement, of what occurs when a nation enshrines a proper earlier than reckoning with the totality of its logic. If autonomy in loss of life is sacrosanct, is there anybody who shouldn’t be helped to die?
Rishad Usmani remembers the primary affected person he killed. She was 77 years previous and a former Ice Capades skater, and she or he had extreme spinal stenosis. Usmani, the girl’s household doctor on Vancouver Island, had tried to speak her out of the choice to die. He would at all times try this, he advised me, when sufferers first requested about medically assisted loss of life, as a result of usually what he discovered was that individuals merely needed to be comfy, to have their ache managed; that once they reckoned, actually reckoned, with the finality of all of it, they realized they didn’t really need euthanasia. However this affected person was positive: She was struggling, not simply from the ache however from the ache remedy too. She needed to die.
On December 13, 2018, Usmani arrived on the girl’s residence within the city of Comox, British Columbia. He was joined by a extra senior doctor, who would supervise the process, and a nurse, who would begin the intravenous line. The affected person lay in a hospital mattress, her sister subsequent to her, holding her hand. Usmani requested her a closing time if she was positive; she stated she was. He administered 10 milligrams of midazolam, a fast-acting sedative, then 40 milligrams of lidocaine to numb the vein in preparation for the 1,000 milligrams of propofol, which might induce a deep coma. Lastly he injected 200 milligrams of a paralytic agent known as rocuronium, which might carry an finish to respiratory, in the end inflicting the guts to cease.
Usmani drew his stethoscope to the girl’s chest and listened. To his quiet alarm, he might hear the guts nonetheless beating. In truth, because the seconds handed, it appeared to be quickening. He glanced at his supervisor. The place had he tousled? However as quickly as they locked eyes, he understood: He was listening to his personal heartbeat.
Many clinicians in Canada who’ve offered medical help in dying have a narrative like this, concerning the tangle of nerves and uncertainties that attended their first case. Dying itself is one thing each clinician is aware of intimately, the grief and pallor and paperwork of it. To work in medication is to step every day into the worst days of different individuals’s lives. However approaching loss of life as a process, as one thing to be scheduled over Outlook, took some getting used to. In Canada, it’s not a novel and memorable occasion. As of 2023, the final 12 months for which information can be found, some 60,300 Canadians had been legally helped to their loss of life by clinicians. In Quebec, greater than 7 p.c of all deaths are by euthanasia—the best fee of any jurisdiction on the planet. “I’ve two or three provisions each week now, and it’s persevering with to go up yearly,” Claude Rivard, a household physician in suburban Montreal, advised me.
Rivard has so far offered for greater than 600 sufferers and helps prepare clinicians new to MAID. This spring, I watched from the again of a small classroom in a Vancouver hospital as Rivard led a workshop on intraosseous infusion—administering medicine straight into the bone marrow, a helpful talent for MAID clinicians, Rivard defined, within the occasion of IV failure. Organized on absorbent pads throughout the again row of tables had been eight pig knuckles, bulbous and pink. After a PowerPoint presentation, the dozen or so attendees took turns with completely different injection gadgets, from the primitive (handbook needles) to the trendy (bone-injection weapons). Arms cramped round hole metal needles because the workshop attendees struggled to twist and drive the instruments residence. This was the very last thing, the clinicians later agreed, that sufferers would need to see as they lay attempting to die. Practitioners wanted to be taught. “Each element issues,” Rivard advised the category; he most popular the bone-injection gun himself.

Johnny C. Y. Lam for The Atlantic
Claude Rivard at his residence close to Montreal
The main points of the assisted-death expertise have develop into a preoccupation of Canadian life. Sufferers meticulously orchestrate their closing moments, planning celebrations round them: weekend home events earlier than a Sunday-night euthanasia within the backyard; a Catholic priest to ship final rites; extended-family renditions of “Auld Lang Syne” on the bedside. For $10.99, you’ll be able to design your MAID expertise with the assistance of the Be Ceremonial app; prompt rituals embody a narrative altar, a forgiveness ceremony, and the amassing of tears from witnesses. On the Disrupting Dying podcast, hosted by an educator and a social employee in Ontario, visitors share concepts on topics akin to normalizing the MAID course of for youngsters going through the loss of life of an grownup of their life—a pajama celebration at a funeral residence; portray a coffin in a schoolyard.
Autonomy, alternative, management: These are the values that discovered buy with the good majority of Canadians in February 2015, when, in a case spearheaded by the British Columbia Civil Liberties Affiliation, the supreme courtroom of Canada unanimously overturned the nation’s prison ban on medically assisted loss of life. For advocates, the victory had been a long time within the making—the end result of a marketing campaign that had grown in fervor because the Nineties, when Canada’s excessive courtroom narrowly dominated towards physician-assisted loss of life in a case introduced by a affected person with amyotrophic lateral sclerosis, or ALS. “We’re speaking a couple of competent individual making a alternative about their loss of life,” one longtime right-to-die activist stated whereas celebrating the brand new ruling. “Don’t entry this alternative in case you don’t need—however steer clear of my loss of life mattress.” A 12 months later, in June 2016, Parliament handed the primary laws formally allowing medical help in dying for eligible adults, putting Canada among the many handful of nations (together with Belgium, Switzerland, and the Netherlands) and U.S. states (Oregon, Vermont, and California, amongst others) that already allowed some model of the follow.
The brand new regulation permitted medical help in dying for adults who had a “grievous and irremediable medical situation” inflicting them “insupportable struggling,” and who confronted a “moderately foreseeable” pure loss of life. To qualify, sufferers wanted two clinicians to log out on their software, and the regulation required a 10-day “reflection interval” earlier than the process might happen. Sufferers might select to die both by euthanasia—having a clinician administer the medicine straight—or, alternatively, by assisted suicide, through which a affected person self-administers a deadly prescription orally. (Nearly all MAID deaths in Canada have been by euthanasia.) When the process was set to start, sufferers had been required to provide closing consent.
The regulation, in different phrases, was premised on the idea of affected person autonomy, however inside slender boundaries. Fairly than power somebody with, say, late-stage most cancers to undergo to the very finish, MAID would enable sufferers to depart on their very own phrases: to expertise a “dignified loss of life,” as proponents known as it. That the brink of eligibility for MAID could be excessive—and stringent—was offered to the general public as self-evident, though the standards themselves had been obscure whenever you seemed carefully. For example, what constituted “moderately foreseeable”? Two months? Two years? Canada’s Division of Justice prompt solely “a time period that isn’t too distant.”
Provincial well being authorities had been left to fill within the blanks. Following the regulation’s passage, docs, nurse practitioners, pharmacists, and attorneys scrambled to attract up the regulatory high quality print for a process that till then had been legally categorized as culpable murder. How ought to the evaluation course of work? What medicine must be used? Notably vexing was the query of whether or not it must be clinicians or sufferers who initiated conversations about assisted loss of life. Some argued that docs and nurses had knowledgeable obligation to broach the topic of MAID with probably eligible sufferers, simply as they might some other “therapy choice.” Others feared that sufferers might interpret this as a suggestion—certainly, feared that speaking about assisted loss of life as a medical therapy, like Lasik surgical procedure or a hip substitute, was harmful in itself.
Early on, plenty of health-care professionals refused to have interaction in any approach with MAID—some due to spiritual beliefs, and others as a result of, of their view, it violated a medical responsibility to “do no hurt.” For a lot of clinicians, the moral and logistical challenges of MAID solely compounded the stress of working inside Canada’s public-health-care system, beset by years of funding cuts and staffing shortages. The median wait time for common surgical procedure is about 22 weeks. For orthopedic surgical procedure, it’s greater than a 12 months. For some sorts of mental-health companies, the wait time may be longer.
As the primary evaluation requests trickled in, even many clinicians who believed strongly in the appropriate to an assisted loss of life had been reluctant to do the precise aiding. Some advised me they agreed to tackle sufferers solely after realizing that nobody else—of their hospital and even their area—was prepared to go first. Matt Kutcher, a doctor on Prince Edward Island, was extra open to MAID than others, however acknowledged the problem of constructing the follow of assisted loss of life just about from scratch. “The fact,” he stated, “is that we had been all simply type of making it up as we went alongside, very cautiously.”


Johnny C. Y. Lam for The Atlantic
Prepared-to-use MAID kits in a hospital vault
On a wet spring night in 2017, Kutcher drove to a farmhouse by the ocean to manage the primary state-sanctioned act of euthanasia in his province. The affected person, Paul Couvrette, had realized about MAID from his spouse, Liana Brittain, in 2015, quickly after the supreme-court choice. He had simply been identified with lung most cancers, and whereas processing this reality within the parking zone of the clinic had turned to his spouse and introduced: “I’m not going to have most cancers. I’m going to kill myself.” Brittain advised her husband this was a bit dramatic. “You understand, expensive, you don’t have to try this,” she remembers responding. “The federal government will do it for you, they usually’ll do it without cost.” Couvrette had marveled on the information, as a result of though he was open to surgical procedure, he had no real interest in chemotherapy or radiation. MAID, Brittain advised me, gave her husband the reduction of a “again door.” By early 2017, the most cancers had unfold to Couvrette’s mind; the 72-year-old turned largely bedridden. He set his MAID process for Might 10—the couple’s wedding ceremony anniversary.
Kutcher and a nurse had agreed to come back early and be part of the prolonged household—kids, a granddaughter—for Couvrette’s closing dinner: seafood chowder and gluten-free biscuits. Solely Brittain would finally be part of Couvrette within the downstairs bed room; the remainder of the household and the couple’s two canines would wait exterior on the seashore. There was a shared understanding, Kutcher recalled, that “this was one thing none of us had skilled earlier than, and we didn’t actually know what we had been in for.” What adopted was a “stunning loss of life”—that was what the native newspaper known as it, Brittain advised me. Couvrette’s final phrases to his spouse got here from their wedding ceremony vows: I’ll love you without end, plus three days.
Kutcher wrestled at first with the sheer strangeness of the expertise—how shortly it was over, packing up his gear in conjunction with a useless man who simply 10 minutes earlier had been speaking with him, very a lot alive. However he went residence believing he had achieved the appropriate factor for his affected person.
For proponents, Couvrette epitomized the perfect MAID candidate, motivated not by an impulsive loss of life want however by a thought of need to reclaim management of his destiny from a terminal illness. The lobbying group Dying With Dignity Canada celebrated Couvrette’s “empowering alternative and journey” as a part of a showcase on its web site of “good deaths” made doable by the brand new regulation. There was additionally the surgeon in Nova Scotia with Parkinson’s who “died the identical approach he lived—on his personal phrases.” And there have been the Toronto couple of their 90s who, in a “dream ending to their storybook romance,” underwent MAID collectively.
Such heartfelt accounts tended to heart on the white, educated, financially steady sufferers who represented the standard MAID recipient. The tales didn’t exactly seize what many clinicians had been discovering additionally to be true: that if dying by MAID was dying with dignity, some deaths felt significantly extra dignified than others. Not everybody has coastal houses or kids and grandchildren who can collect in love and solidarity. This was made clear to Sandy Buchman, a palliative-care doctor in Toronto, throughout one in all his early MAID circumstances, when a affected person, “on their own,” gave closing consent from a mattress on the ground of a rental condominium. Buchman remembers having to kneel subsequent to the mattress within the in any other case empty house to manage the medicine. “It was horrible,” he advised me. “You’ll be able to see how difficult, how terrible, issues may be.”
In 2018, Buchman co-founded a nonprofit group known as MAiDHouse. The intention was to create a “third place” of kinds for individuals who need to die someplace aside from a hospital or at residence. Discovering a location proved tough; many landlords had been resistant. However by 2022, MAiDHouse had leased the house in Toronto from which it operates at the moment. (For safety causes, the situation is just not public.) Tekla Hendrickson, the chief director of MAiDHouse, advised me the house was designed to really feel heat and acquainted but in addition adaptable to the desires of the individual utilizing it: furnishings mild sufficient to rearrange, naked surfaces for flowers or photographs or some other private gadgets. “Typically they’ve champagne, generally they arrive in limos, generally they put on ball robes,” Hendrickson stated. The act of euthanasia itself takes place in a La-Z-Boy-like recliner, with adjoining rooms out there for household and mates who might choose to not witness the process. Based on the MAiDHouse web site, the physique is then transferred to a funeral residence by attendants who arrive in unmarked automobiles and depart “discreetly.”
Since its founding, MAiDHouse has offered house and help for greater than 100 deaths. The group’s homepage shows {a photograph} of dandelion seeds scattering in a delicate wind. A second MAiDHouse location lately opened in Victoria, British Columbia. Within the group’s 2023 annual report, the chair of the board famous that MAiDHouse’s followers on LinkedIn had elevated by 85 p.c; its new Instagram profile was gaining followers too. Extra to the purpose, the variety of provisions carried out at MAiDHouse had doubled over the earlier 12 months—“astounding progress for such a younger group.”
Within the early days of MAID, some clinicians discovered themselves without delay stunned and conflicted by the achievement they skilled in serving to individuals die. Just a few months after the regulation’s passage, Stefanie Inexperienced, whom I’d met on the convention in Vancouver, acknowledged to herself how “upbeat” she’d felt following a current provision—“a bit overrated on adrenaline,” as she later put it in a memoir about her first 12 months offering medical help in loss of life. Inexperienced realized it was gratification she was feeling: A affected person had come to her in immense ache, and she or he had been able to supply reduction. Ultimately, she believed, she had “given a present to a dying man.”
Inexperienced had at first been reluctant to disclose her emotions to anybody, afraid that she is perhaps seen, she recalled, as a “psychopath.” However she did finally open up to a small group of fellow MAID practitioners. Inexperienced and several other colleagues realized that there was a necessity for a proper neighborhood of pros. In 2017, they formally launched the group whose assembly I attended.
There was a time when Madeline Li would have felt completely at residence among the many different clinicians who convened that weekend on the Sheraton. Within the early years of MAID, few physicians exerted extra affect over the brand new regime than Li. The Toronto-based most cancers psychiatrist led the event of the MAID program on the College Well being Community, the biggest teaching-hospital system in Canada, and in 2017 noticed her framework revealed in The New England Journal of Medication.

Tony Luong for The Atlantic
Madeline Li at her workplace in Toronto
It was not lengthy into her follow, nevertheless, that Li’s confidence within the path of her nation’s MAID program started to falter. For all of her experience, not even Li was positive what to do a couple of affected person in his 30s whom she encountered in 2018.
The person had gone to the emergency room complaining of excruciating ache and was finally identified with most cancers. The prognosis was good, a surgeon assured him, with a 65 p.c likelihood of a remedy. However the man stated he didn’t need therapy; he needed MAID. Startled, the surgeon referred him to a medical oncologist to debate chemo; maybe the person simply didn’t need surgical procedure. The affected person proceeded to inform the medical oncologist that he didn’t need therapy of any variety; he needed MAID. He stated the identical factor to a radiation oncologist, a palliative-care doctor, and a psychiatrist, earlier than lastly complaining to the patient-relations division that the hospital was barring his entry to MAID. Li organized to fulfill with him.
Canada’s MAID regulation defines a “grievous and irremediable medical situation” partially as a “severe and incurable sickness, illness, or incapacity.” As for what constitutes incurability, nevertheless, the regulation says nothing—and of the varied textual ambiguities that brought on anxiousness for clinicians early on, this one ranked close to the highest. Did “incurable” imply a scarcity of any out there therapy? Did it imply the chance of an out there therapy not working? Outstanding MAID advocates put forth what quickly turned the predominant interpretation: A medical situation was incurable if it couldn’t be cured by means acceptable to the affected person.
This had made sense to Li. If an aged girl with power myelogenous leukemia had no want to endure a extremely poisonous course of chemo and radiation, why ought to she be compelled to? However right here was a younger man with a probable curable most cancers who however was adamant about dying. “I imply, he was so, so clear,” Li advised me. “I talked to him about What in case you had a one hundred pc likelihood? Would you need therapy? And he stated no.” He didn’t need to undergo by means of the therapy or the negative effects, he defined; simply having a colonoscopy had traumatized him. When Li assured the person that they may deal with the negative effects, he stated she wasn’t understanding him: Sure, they may give him remedy for the ache, however then he must first expertise the ache. He didn’t need to expertise the ache.
What was Li left with? Based on prevailing requirements, the person’s refusal to try therapy rendered his illness incurable and his pure loss of life was moderately foreseeable. He met the eligibility standards as Li understood them. However the entire thing appeared fallacious to her. In search of recommendation, she described the fundamentals of the case in a non-public e-mail group for MAID practitioners underneath the heading “Eligible, however Affordable?” “And what was very clear to me from the replies I bought,” Li advised me, “is that many individuals haven’t any moral or medical qualms about this—that it’s all a couple of affected person’s autonomy, and if a affected person needs this, it’s less than us to guage. We must always present.”
And so she did. She regretted her choice virtually as quickly as the person’s coronary heart stopped beating. “What I’ve realized since is: Eligible doesn’t imply it is best to present MAID,” Li advised me. “You may be eligible as a result of the regulation is so stuffed with holes, however that doesn’t imply it clinically is sensible.” Li not interprets “incurable” as on the sole discretion of the affected person. The issue, she feels, is that the regulation permits such a large spectrum of interpretations to start with. Many selections about life and loss of life activate the private values of practitioners and sufferers quite than on any goal medical standards.
By 2020, Li had overseen a whole lot of MAID circumstances, about 95 p.c of which had been “very easy,” she stated. They concerned individuals who had terminal circumstances and needed the identical management in loss of life as they’d loved in life. It was the 5 p.c that nervous her—not simply the younger man, however susceptible individuals extra usually, whom the safeguards had probably failed. Sufferers whose solely “terminal situation,” actually, was age. Li recalled an particularly divisive early case for her group involving an aged girl who’d fractured her hip. She understood that the remainder of her life would imply changing into solely weaker and enduring extra falls, and she or he “simply wasn’t going to have it.” The girl was permitted for MAID on the premise of frailty.
Li had tried to grasp the assessor’s reasoning. Based on an actuarial desk, the girl, given her age and medical circumstances, had a life expectancy of 5 or 6 extra years. However what if the girl had been barely youthful and the quantity was nearer to eight years—would the clinician have permitted her then? “And so they stated, effectively, they weren’t positive, and that’s my level,” Li defined. “There’s no customary right here; it’s simply type of as much as you.” The idea of a “accomplished life, or being bored with life,” as ample for MAID is “controversial in Europe and theoretically not authorized in Canada,” Li stated. “However the fact is, it is authorized in Canada. It at all times has been, and it’s occurring in these frailty circumstances.”
Li helps medical help in dying when acceptable. What troubles her is the federal authorities’s deferring of duty in managing it—establishing ideas, setting requirements, imposing boundaries. She believes most physicians in Canada share her “muddy center” place. However that place, she stated, can be “essentially the most silent.”
In 2014, when the query of medically assisted loss of life had come earlier than Canada’s supreme courtroom, Etienne Montero, a civil-law professor and on the time the president of the European Institute of Bioethics, warned in testimony that the follow of euthanasia, as soon as authorized, was unattainable to manage. Montero had been retained by the lawyer common of Canada to debate the expertise of assisted loss of life in Belgium—how a regime that had begun with “extraordinarily strict” standards had steadily advanced, by means of free interpretations and lax enforcement, to accommodate most of the very sufferers it had as soon as pledged to guard. When a affected person’s autonomy is paramount, Montero argued, growth is inevitable: “In the end, a affected person’s repeated want will take priority over strict statutory circumstances.” Ultimately, the Canadian justices had been unmoved; Belgium’s “permissive” system, they contended, was the “product of a really completely different medico-legal tradition” and subsequently provided “little perception into how a Canadian regime would possibly function.” In a way, this was right: It took Belgium greater than 20 years to achieve an assisted-death fee of three p.c. Canada wanted solely 5.
On reflection, the growth of MAID would appear to have been inevitable; Justin Trudeau, then Canada’s prime minister, stated as a lot again in 2016, when he known as his nation’s newly handed MAID regulation “a giant first step” in what could be an “evolution.” 5 years later, in March 2021, the federal government enacted a brand new two-track system of eligibility, enjoyable present safeguards and increasing MAID to a broader swath of Canadians. Sufferers permitted for an assisted loss of life underneath Observe 1, because it was now known as—that means the unique end-of-life context—had been not required to attend 10 days earlier than receiving MAID; they may die on the day of approval. Observe 2, in the meantime, legalized MAID for adults whose deaths weren’t moderately foreseeable—individuals affected by power ache, for instance, or from sure neurological problems. Though value financial savings have by no means been talked about as an express rationale for growth, the parliamentary funds workplace anticipated annual financial savings in health-care prices of almost $150 million on account of the expanded MAID regime.
The 2021 regulation did present for added safeguards distinctive to Observe 2. Assessors had to make sure that candidates gave “severe consideration”—a phrase left undefined—to “cheap and out there means” to alleviate their struggling. As well as, they needed to affirm that the sufferers had been directed towards such choices. Observe 2 assessments had been additionally required to span at the very least 90 days. For any MAID evaluation, clinicians have to be glad not solely {that a} affected person’s struggling is enduring and insupportable, however that it’s a operate of a bodily medical situation quite than psychological sickness, say, or monetary instability. Struggling is rarely completely reducible, after all—a crisp research in trigger and impact. However when a affected person is already dying, the function of bodily illness isn’t often a thriller, both.
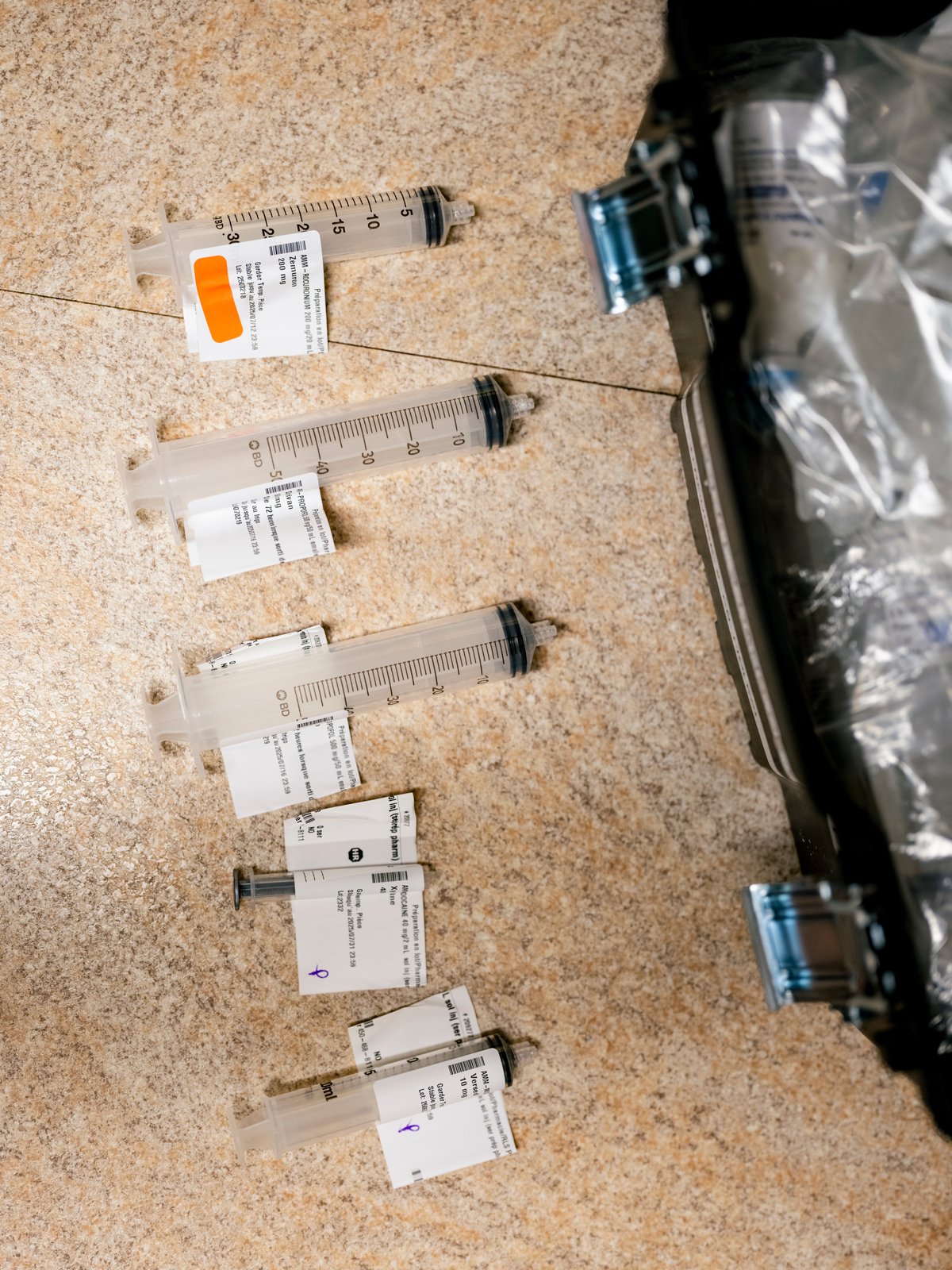
Johnny C. Y. Lam for The Atlantic
Depleted syringes after a MAID provision
Observe 2 launched an internet of ethical complexities and medical calls for. For a lot of practitioners, one main new issue was the sheer period of time required to grasp why the individual earlier than them—not terminally unwell—was asking, at that individual second, to die. Clinicians must untangle the bodily expertise of power sickness and incapacity from the structural inequities and mental-health struggles that usually attend it. In a system the place entry to social helps and medical companies varies so broadly, this was no small problem, and lots of clinicians in the end selected to not develop their follow to incorporate Observe 2 sufferers.
There is no such thing as a clear official information on what number of clinicians are prepared to tackle Observe 2 circumstances. The federal government’s most up-to-date info signifies that, in 2023, out of two,200 MAID practitioners total, a mere 89 had been chargeable for about 30 p.c of all Observe 2 provisions. Jonathan Reggler, a household doctor on Vancouver Island, is amongst that small group. He overtly acknowledges the challenges concerned in assessing Observe 2 sufferers, in addition to the essential “discomfort” that comes with ending the life of somebody who is just not actually dying. “I can consider circumstances that I’ve handled the place you’re actually asking your self, Why? ” he advised me. “Why now? Why is it that this cluster of issues is inflicting you such misery the place one other individual wouldn’t be distressed? ”
But Reggler feels responsibility sure to maneuver past his private discomfort. As he defined it, “When you settle for that individuals should have autonomy—when you settle for that life is just not sacred and one thing that may solely be taken by God, a being I don’t consider in—then, in case you’re in that work, a few of us should go ahead and say, ‘We’ll do it.’ ”
For some MAID practitioners, nevertheless, it took encountering an eligible affected person for them to appreciate the true extent of their unease with Observe 2. One doctor, who requested anonymity as a result of he was not approved by his hospital to talk publicly, recalled assessing a affected person of their 30s with nerve injury. The ache was such that they couldn’t go exterior; even the contact of a breeze would inflame it. “They’d seen each type of specialist,” he stated. The affected person had tried nontraditional therapies too—acupuncture, Reiki, “every thing.” Because the doctor noticed it, the affected person’s situation was severe and incurable, it was inflicting insupportable struggling, and the struggling couldn’t appear to be relieved. “I went by means of the entire tick containers, and by the letter of the regulation, they clearly met the standards for all of this stuff, proper? That stated, I felt a bit bit queasy.” The affected person was younger, with a situation that isn’t terminal and is often treatable. However “I didn’t really feel it was my place to inform them no.”
He was not comfy doing the process himself, nevertheless. He recalled telling the MAID workplace in his area, “Look, I did the evaluation. The affected person meets the standards. However I simply can’t—I can’t do that.” One other clinician stepped in.
In 2023, Observe 2 accounted for 622 MAID deaths in Canada—simply over 4 p.c of circumstances, up from 3.5 p.c in 2022. Whether or not the proportion continues to rise is anybody’s guess. Some argue that primary-care suppliers are greatest positioned to barter the complexities of Observe 2 circumstances, given their familiarity with the affected person making the request—their household state of affairs, medical historical past, social circumstances. That is how assisted loss of life is usually approached in different nations, together with Belgium and the Netherlands. However in Canada, the system largely developed across the MAID coordination facilities assembled within the provinces, full with 1-800 numbers for self-referrals. The result’s that MAID assessors usually haven’t any preexisting relationship with the sufferers they’re assessing.
How do you navigate, then, the hidden corridors of a stranger’s struggling? Claude Rivard advised me a couple of Observe 2 affected person who had known as to cancel his scheduled euthanasia. On account of a bike accident, the person couldn’t stroll; now blind, he was residing in a long-term-care facility and infrequently had guests; he had been persistent in his request for MAID. However when his household realized that he’d utilized and been permitted, they began visiting him once more. “And it modified every thing,” Rivard stated. He was in touch together with his kids once more. He was in touch together with his ex-wife once more. “He determined, ‘No, I nonetheless have pleasure in life, as a result of the household, the children are coming; even when I can’t see them, I can contact them, and I can discuss to them, so I’m altering my thoughts.’ ”
I requested Rivard whether or not this flip of occasions—the obvious plasticity of the person’s need to die—had given him pause about approving the affected person for MAID within the first place. In no way, he stated. “I had no management on what the household was going to do.”
Among the opposition to MAID in Canada is spiritual in character. The Catholic Church condemns euthanasia, although Church affect in Canada, as elsewhere, has waned dramatically, notably the place it was as soon as strongest, in Quebec. However from the outset there have been different considerations, chief amongst them the fear that assisted loss of life, initially approved for one class of affected person, would finally develop into authorized for an important many others too. Nationwide disability-rights teams warned that Canadians with bodily and mental disabilities—individuals whose lives had been already undervalued in society, and of whom 17 p.c stay in poverty—could be at specific danger. As assisted loss of life turned “sanitized,” one group argued, “an increasing number of might be inspired to decide on this feature, additional entrenching the ‘higher off useless’ message in public consciousness.”

Johnny C. Y. Lam for The Atlantic
At a hospital in Quebec, a pharmacist prepares the medicine utilized in euthanasia.
For these critics, the “moderately foreseeable” loss of life requirement had been the solitary comfort in an in any other case misplaced constitutional battle. The elimination of that safety with the creation of Observe 2 bolstered their conviction that MAID would lead to Canada’s most marginalized residents being subtly coerced into untimely loss of life. Canadian officers acknowledged these considerations—“We all know that in some locations in our nation, it’s simpler to entry MAID than it’s to get a wheelchair,” Carla Qualtrough, the disability-inclusion minister, admitted in 2020—however reiterated that socioeconomic struggling was not a authorized foundation for MAID. Justin Trudeau took pains to guarantee the general public that sufferers weren’t being backed into assisted loss of life due to their lack of ability to afford correct housing, say, or get well timed entry to medical care. It “merely isn’t one thing that finally ends up occurring,” he stated.
Sathya Dhara Kovac, of Winnipeg, knew in any other case. Earlier than dying by MAID in 2022, on the age of 44, Kovac wrote her personal obituary. She defined that life with ALS had “not been simple”; it was, so far as sicknesses went, a “shitty” one. However the sickness itself was not the rationale she needed to die. Kovac advised the native press previous to being euthanized that she had fought unsuccessfully to get satisfactory home-care companies; she wanted greater than the 55 hours every week lined by the province, couldn’t afford the price of a non-public company to deal with the stability, and didn’t need to be relegated to a long-term-care facility. “In the end it was not a genetic illness that took me out, it was a system,” Kovac wrote. “I might have had extra time if I had extra assist.”
Earlier this spring, I met in Vancouver with Marcia Doherty; she was permitted for Observe 2 MAID shortly after it was legalized, 4 years in the past. The 57-year-old has suffered for many of her life from advanced power sicknesses, together with myalgic encephalomyelitis, fibromyalgia, and Epstein-Barr virus. Her every day expertise of ache is so complete that it’s best captured when it comes to what doesn’t damage (the information of her ears; generally the tip of her nostril) versus all of the locations that do. But on the core of her struggling is just not solely the ache itself, Doherty advised me; it’s that, because the years go by, she will be able to’t afford the price of managing it. Solely a fraction of the therapies she depends on are lined by her province’s health-care plan, and with month-to-month incapacity help her solely constant revenue, she is overwhelmed with medical debt. Doherty understands that sometime, the stress might merely develop into an excessive amount of. “I didn’t apply for MAID as a result of I need to be useless,” she advised me. “I utilized for MAID on ruthless practicality.”
It’s obscure MAID in such circumstances as a triumphant act of autonomy—as if the state, by facilitating loss of life the place it has failed to supply satisfactory sources to stay, has in some way given its most susceptible residents the dignity of alternative. In January 2024, a quadriplegic man named Normand Meunier entered a Quebec hospital with a respiratory an infection; after 4 days confined to an emergency-room stretcher, unable to safe a correct mattress regardless of his companion’s pleas, he developed a painful bedsore that led him to use for MAID. “I don’t need to be a burden,” he advised Radio-Canada the day earlier than he was euthanized, that March.
Almost half of all Canadians who’ve died by MAID seen themselves as a burden on household and mates. For some disabled residents, the provision of assisted loss of life has sowed doubt about how the medical institution itself sees them—about whether or not their lives are actually thought of worthy of saving. Within the fall of 2022, a 49-year-old Nova Scotia girl who’s bodily disabled and had lately been identified with breast most cancers was readying for a lifesaving mastectomy when a member of her surgical group started working by means of a listing of pre-op questions on her drugs and the final time she ate—and was she accustomed to medical help in dying? The girl advised me she felt instantly and aware of her physique, the tissue-thin robe that wouldn’t shut. “It left me feeling like possibly I must be second-guessing my choice,” she recalled. “It was the factor I used to be interested by as I went underneath; after I awoke, it was the primary thought in my head.” Fifteen months later, when the girl returned for a second mastectomy, she was once more requested if she was conscious of MAID. As we speak she nonetheless wonders if, had been she not disabled, the query would even have been requested. Gus Grant, the registrar and CEO of the School of Physicians and Surgeons of Nova Scotia, has stated that the timing of the queries to this girl was “clearly inappropriate and insensitive,” however he additionally emphasised that “there’s a distinction between elevating the subject of discussing consciousness about MAID, and doable eligibility, from providing MAID.”
And but there may be additionally a purpose why, in some nations, clinicians are both expressly prohibited or usually discouraged from initiating conversations about assisted loss of life. Nonetheless sensitively the topic is broached, loss of life by no means presents itself neutrally; to treat the road between an “supply” and a easy recitation of data as in some way self-evident is to disregard this reality, in addition to the ability imbalance that freights a well being skilled’s each gesture with profound that means. Maybe the now-suspended Veterans Affairs caseworker who, in 2022, was discovered by the division to have “inappropriately raised” MAID with a number of service members had meant no hurt. However in line with testimony, one fight veteran was so shaken by the alternate—he had known as in search of help for his illnesses and was not suicidal, however was advised that MAID was preferable to “blowing your brains out”—that he left the nation.
In 2023, Kathrin Mentler, who lives with concurrent psychological and bodily disabilities, together with rheumatoid arthritis and different types of power ache, arrived at Vancouver Common Hospital asking for assist amid a suicidal disaster. Mentler has acknowledged in a sworn affidavit that the hospital clinician who carried out the consumption advised her that though they may contact the on-call psychiatrist, no beds had been out there within the unit. The clinician then requested if Mentler had ever thought of MAID, describing it as a “peaceable” course of in contrast together with her current suicide try by way of overdose, for which she’d been hospitalized. Mentler stated that she left the hospital in a “panic,” and that the encounter had validated a lot of her worst fears: that she was a “burden” on an overtaxed system and that it could be “cheap” for her to need to die. (In response to press stories about Mentler’s expertise, the regional well being authority stated that the dialog was a part of a “medical analysis” to evaluate suicide danger and that workers are required to “discover all out there care choices” with sufferers.)
MAID advocates dispute the cost that disabled Canadians are being quietly or overtly pressured to think about assisted loss of life, calling it a fantasy generated by what they view as sensationalized accounts within the press; in parliamentary hearings, lawmakers, citing federal information, have emphasised that “solely a small quantity” of MAID recipients are unable to entry the medical companies and social helps they require. Even so, this previous March, the United Nations Committee on the Rights of Individuals With Disabilities formally known as for the repeal of Observe 2 MAID in Canada—arguing that the federal authorities had “basically modified” the premise of assisted dying on the premise of “detrimental, ableist perceptions of the standard and worth” of disabled lives, with out addressing the systemic inequalities that amplify their perceived struggling.
Marcia Doherty agrees that it ought to by no means have come to this: her nation resolving to help her and different disabled residents extra in loss of life than in life. She is livid that she has been “allowed to deteriorate,” regardless of advocating for herself earlier than each company and official able to effecting change. However she is adamantly against any repeal of Observe 2. She expressed a sentiment I heard from others in my reporting: that the “reduction” of figuring out an assisted loss of life is on the market to her, ought to the despair develop into insufferable, has empowered her within the battle to stay.
Doherty might sometime determine to entry MAID. However she doesn’t need anybody ever to say she “selected” it.
Ellen Wiebe by no means had reservations about taking up Observe 2 circumstances—certainly, in contrast to most clinicians, she by no means had reservations about offering MAID in any respect. The Vancouver-based household doctor had lengthy been comfy with controversy, having spent the majority of her 4 a long time in medication as an abortion supplier. As Wiebe noticed it, MAID was completely in line with her “human-rights-focused” profession. Over the previous 9 years, she has euthanized greater than 430 sufferers and develop into one of many world’s most outspoken champions of MAID. As we speak, whereas just about all of her colleagues depend on referrals from MAID coordination facilities, Wiebe repeatedly receives requests straight from sufferers. Coordinators additionally name her once they have a affected person whose earlier MAID requests had been rejected. (There is no such thing as a restrict to what number of occasions an individual can apply for MAID.) “As a result of I’m me, you understand, they ship these all the way down to Ellen Wiebe,” she advised me. I requested her what she meant by that. “My popularity,” she replied.
In the summertime of 2024, Wiebe heard from a 53-year-old girl in Alberta who was experiencing acute psychiatric misery—“the horrors,” the affected person known as them—compounded by her response to, after which withdrawal from, an antipsychotic drug she was prescribed for sleep. Not one of the girl’s docs would facilitate her need to die. This was when, in line with the model of occasions the girl’s common-law husband would later undergo British Columbia’s supreme courtroom, she searched on-line for options and got here throughout Wiebe. On the finish of their first assembly, a Zoom name, Wiebe stated she would approve the girl for the process. On her formal software, the girl gave “akathisia”—a motion dysfunction characterised by intense emotions of inside restlessness and an lack of ability to sit down nonetheless, generally attributable to withdrawal from antipsychotic remedy—as her purpose for requesting an assisted loss of life. Based on courtroom filings, nobody the girl knew was prepared to witness her signal the applying kind, because the regulation requires, so Wiebe had a volunteer at her clinic accomplish that over Zoom. And since the girl nonetheless wanted one other doctor or nurse practitioner to declare her eligible, Wiebe organized for Elizabeth Whynot, a fellow household doctor in Vancouver, to supply the second evaluation. The affected person was permitted for MAID after a video name, and the process was set for October 27, 2024, in Wiebe’s clinic.
Following the approval, detailed within the courtroom filings, the Alberta girl had one other Zoom name with Wiebe; this time, her husband joined the dialog. He had considerations, particularly as to how akathisia certified as “irremediable.” Specialists had assured the girl that if she dedicated to the gradual tapering protocol they’d prescribed, she might very seemingly count on reduction inside months. The husband additionally nervous that Wiebe hadn’t sufficiently thought of his spouse’s unresolved mental-health points, and whether or not she was succesful, in her current state, of giving actually knowledgeable consent. The day earlier than his spouse was scheduled to die, he petitioned a Vancouver choose to halt the process, arguing that Wiebe had negligently permitted the girl on the premise of a situation that didn’t qualify for MAID. In a broadly publicized choice, the following morning the choose issued a last-minute injunction blocking Wiebe or some other clinician from finishing up the girl’s loss of life as scheduled. “I can solely think about the ache she has been experiencing, and I acknowledge that this injunction will seemingly solely make that worse,” the choose wrote. However there was an “debatable case,” he concluded, as as to if the standards for MAID had been “correctly utilized within the circumstances.” The husband didn’t search a brand new injunction after the non permanent order expired, and in January, he withdrew the lawsuit altogether. Wiebe wouldn’t touch upon the case aside from to say she has by no means violated MAID legal guidelines and doesn’t know of any supplier who has. The lawyer who had represented the husband stated she couldn’t touch upon whether or not the girl continues to be alive.

Jennilee Marigomen for The Atlantic
Ellen Wiebe at her workplace in Vancouver
Quite a few related lawsuits have been filed in recent times as Canadians come to phrases with the hole oversight of MAID. As a result of no formal process exists for difficult an approval prematurely of a provision, many involved members of the family see little alternative however to take a beloved one to courtroom to attempt to halt a scheduled loss of life. What oversight does exist takes place on the provincial or territorial degree, and solely after the actual fact. Protocols differ considerably throughout jurisdictions. In Ontario, the chief coroner’s workplace oversees a system through which all Observe 2 circumstances are mechanically referred to a multidisciplinary committee for postmortem scrutiny. Since 2018, the coroner’s workplace has recognized greater than 480 compliance points involving federal and provincial MAID insurance policies, together with clinicians failing to seek the advice of with an knowledgeable of their affected person’s situation previous to approval—a key Observe 2 safeguard—and utilizing the fallacious medicine in a provision. The workplace’s death-review committee periodically publishes summaries of specific circumstances, for each Observe 1 and Observe 2, to “generate dialogue” for “sensible enchancment.”
There was, for instance, the case of Mr. C, a person in his 70s who, in 2024, requested MAID whereas receiving in-hospital palliative look after metastatic most cancers. It ought to have been a simple Observe 1 case. However two days after his request, in line with the committee’s report, the person skilled sharp cognitive decline and misplaced the power to speak, his eyes opening solely in response to painful stimuli. His palliative-care group deemed him incapable of consenting to health-care selections, together with closing permission for MAID. Regardless of that conclusion, a MAID clinician proceeded with the evaluation, “vigorously” rousing the person to ask if he nonetheless needed euthanasia (to which the person mouthed “sure”), after which withholding the person’s ache remedy till he appeared “extra alert.” After confirming the person’s needs by way of “brief verbal statements” and “head nods and blinking,” the assessor permitted him for MAID; with sign-off from a second clinician, and a closing consent from Mr. C mouthing “sure,” he was euthanized.
Had this affected person clearly consented to his loss of life? Discovering no documentation of a “rigorous analysis of capability,” the death-review committee expressed “considerations” concerning the course of. The implication would appear startling—in a regime animated at its core by affected person autonomy, a person was not credibly discovered to have exercised his personal. But Mr. C’s loss of life was decreased primarily to a matter of educational inquiry, a possibility for “classes realized.” Of the a whole lot of irregularities flagged through the years by the coroner’s workplace, virtually all have been handled by means of an “Casual Dialog,” an “Academic E mail,” or a “Discover E mail,” relying on their severity. Particular sanctions will not be made public. No case has ever been referred to regulation enforcement for investigation.
Wiebe acknowledged that a number of complaints have been filed towards her through the years however famous that she has by no means been discovered responsible of wrongdoing. “And if a lawyer says, ‘Oh—I disagreed with a few of these issues,’ I’d say, ‘Effectively, they didn’t put attorneys in control of this.’ ” She laughed. “We had been those trusted with the safeguards.” And the regulation was clear, Wiebe stated: “If the assessor”—that means herself—“believes that they qualify, then I’m not responsible of a criminal offense.”
Regardless of all of the questions surrounding Observe 2, Canada is continuing with the growth of MAID to further classes of sufferers whereas gauging public curiosity in much more. As early as 2016, the federal authorities had agreed to launch exploratory investigations into the doable future provision of MAID for individuals whose sole underlying medical situation is a psychological dysfunction, in addition to to “mature minors,” individuals youthful than 18 who’re “deemed to have requisite decision-making capability.” The federal government additionally pledged to think about “advance requests”—that’s, permitting individuals to consent now to obtain MAID at some specified future level when their sickness renders them incapable of constructing or affirming the choice to die. In the meantime, the Quebec School of Physicians has raised the opportunity of legalizing euthanasia for infants born with “extreme malformations,” a uncommon follow at the moment authorized solely within the Netherlands, the primary nation to undertake it since Nazi Germany did so in 1939.
As a part of Observe 2 laws in 2021, lawmakers prolonged eligibility—to take impact sooner or later sooner or later—to Canadians affected by psychological sickness alone. This, regardless of the submissions of most of the nation’s high psychiatric and mental-health organizations that no evidence-based customary exists for figuring out whether or not a psychiatric situation is irremediable. Quite a few specialists additionally shared considerations about whether or not it was doable to credibly distinguish between suicidal ideation and a need for MAID.
After a number of contentious delays, MAID for psychological sickness is now set to take impact in 2027; authorities have been tasked within the meantime with determining how MAID ought to really be utilized in such circumstances. The controversy has produced hundreds of pages of particular stories and parliamentary testimony. What all sides do agree on is that, in follow, psychological problems are already a daily function of Canada’s MAID regime. At one listening to, Mona Gupta, a psychiatrist and the chair of an knowledgeable panel charged with recommending protocols and safeguards for psychiatric MAID, famous pointedly that “individuals with psychological problems are requesting and accessing MAID now.” They embody sufferers whose requests are “largely motivated by their psychological dysfunction however who occur to have one other qualifying situation,” in addition to these with “lengthy histories of suicidality” or questionable decision-making capability. They might even be poor and homeless and have little interplay with the health-care system. However regardless of the case, Gupta stated, relating to navigating the advanced intersection of MAID and psychological sickness, “assessors and health-care suppliers already do that.”
The argument was meant to assuage considerations about medical readiness. For critics, nevertheless, it solely bolstered a perception that, in some circumstances, bodily circumstances are merely getting used to bear the authorized weight of a unique, ineligible foundation for MAID, together with psychological problems. In one in all Canada’s extra controversial circumstances, a 61-year-old man named Alan Nichols, who had a historical past of melancholy and different circumstances, utilized for MAID in 2019 whereas on suicide watch at a British Columbia hospital. Just a few weeks later, he was euthanized on the premise of “listening to loss.”
As Canadians await the rollout of psychiatric MAID, Parliament’s Particular Joint Committee on Medical Help in Dying has formally really helpful increasing MAID entry to mature minors. Within the committee’s 2023 report, following a collection of hearings, lawmakers acknowledged the varied elements that would have an effect on younger individuals’s capability to guage their circumstances—for one, the adolescent mind’s removed from totally developed colleges for “danger evaluation and decision-making.” However they famous that, in line with a number of parliamentary witnesses, kids with severe medical circumstances “are likely to possess an unusual degree of maturity.” The committee suggested that MAID be restricted (“at this stage”) to minors with moderately foreseeable pure deaths, and endorsed a requirement for “parental session,” however not parental consent. As a lawyer with the School of Physicians and Surgeons of Saskatchewan advised the committee, “Mother and father could also be reluctant to consent to the loss of life of their baby.”
Whether or not Canadian officers will finally add mature minors to the eligibility listing stays unclear. In the intervening time, their consideration is essentially centered on a unique class of growth. Final 12 months, the province of Quebec took the following step in what some regard because the “pure evolution” of MAID: the honoring of advance requests to be euthanized. Beneath the Quebec regulation, sufferers within the province with cognitive circumstances akin to Alzheimer’s can outline a threshold they don’t want to cross. Some individuals would possibly request to die once they not acknowledge their kids, for instance; others would possibly point out incontinence as a benchmark. When the brink appears to have been reached, maybe after an alert from a “trusted third celebration,” a MAID practitioner determines whether or not the affected person is certainly struggling intolerably in line with the phrases of the advance request. Since 2016, public demand for this growth has been regular, fueled by the testimonies of those that have watched family members endure the total course of dementia and don’t need to undergo the identical destiny.
In parliamentary hearings, Quebec officers have mentioned the potential drawback of “nice dementia,” acknowledging that it is perhaps tough for a supplier to euthanize somebody who “appears glad” and “completely doesn’t keep in mind” consenting to an assisted loss of life earlier of their sickness. Quebec officers have additionally mentioned the problem of resistance. The Netherlands, the one different jurisdiction the place euthanizing an incapable however acutely aware individual on account of an advance request is authorized, provides an instance of what MAID in such a circumstance might seem like.
In 2016, a geriatrician within the Netherlands euthanized an aged girl with Alzheimer’s who, 4 years earlier, shortly after being identified, had suggested that she needed to die when she was “not in a position to stay at residence.” Finally, the girl was admitted to a nursing residence, and her husband duly requested the ability’s geriatrician to provoke MAID. The geriatrician, together with two different docs, agreed that the girl was “struggling hopelessly and intolerably.” On the day of the euthanasia, the geriatrician determined so as to add a sedative surreptitiously to the girl’s espresso; it was given to “forestall a battle,” the physician would later clarify, and surreptitiously as a result of the girl would have “requested questions” and “refused to take it.” However because the injections started, the girl reacted and tried to sit down up. Her household helped maintain her down till the process was over and she or he was useless. The case prompted the primary prison investigation underneath the nation’s euthanasia regulation. The doctor was acquitted by a district courtroom in 2019, and that call was upheld by the Dutch supreme courtroom the next 12 months.
In Quebec, greater than 100 advance requests have been filed; in line with a number of sources, at the very least one has been carried out. The regulation at the moment states that any signal of refusal “have to be revered”; on the identical time, if the clinician determines that expressions of resistance are “behavioural signs” of a affected person’s sickness, and never essentially an precise objection to receiving MAID, the euthanasia can proceed anyway. The Canadian Affiliation of MAiD Assessors and Suppliers has acknowledged that “pre-sedating the individual with drugs akin to benzodiazepines could also be warranted to keep away from potential behaviours which will consequence from misunderstanding.”
Laurent Boisvert, an emergency doctor in Montreal who has euthanized some 600 individuals since 2015, advised me that he has so far helped seven sufferers, lately identified with Alzheimer’s, to file advance requests, and that they included clear directions on what he’s to do within the occasion of resistance. He’s not involved about probably encountering glad dementia. “It doesn’t exist,” he stated.
The Canadian authorities had tried, within the early years of MAID, to forecast the nation’s demand for assisted loss of life. The primary projection, in 2018, was that Canada’s MAID fee would obtain a “regular state” of two p.c of complete deaths; then, in 2022, federal officers estimated that the speed would stabilize at 4 p.c by 2033. After Canada blew previous each numbers—the latter, 11 years forward of schedule—officers merely stopped publishing predictions.
And but it was by no means clear how Canadians had been meant to grasp their nation’s assisted-death fee: whether or not, within the authorities’s view, there may be such a factor as an excessive amount of MAID. In parliamentary hearings, federal officers have indicated {that a} nationwide fee of seven p.c—the speed already reached in Quebec—is perhaps probably “regarding” and “clever and prudent to look into,” however didn’t elaborate additional. If Canadian leaders really feel viscerally troubled by a sure prevalence of euthanasia, they appear reluctant to clarify why.
The unique assumption was that euthanasia in Canada would comply with roughly the identical trajectory that euthanasia had adopted in Belgium and the Netherlands. However even underneath these permissive regimes, the regulation requires that sufferers exhaust all out there therapy choices earlier than in search of euthanasia. In Canada, the place making certain entry has at all times been paramount, such a requirement was regarded as an excessive amount of of an infringement on affected person autonomy. Though Observe 2 requires that sufferers be told of doable different technique of assuaging their struggling, it doesn’t require that these choices really be made out there. Final 12 months, the Quebec authorities introduced plans to spend almost $1 million on a research of why so many individuals within the province are selecting to die by euthanasia. The announcement got here shortly after Michel Bureau, who heads Quebec’s MAID-oversight committee, expressed concern that assisted loss of life is not seen as an choice of final resort. However had it ever been?
It doesn’t really feel fairly proper to say that Canada slid down a slippery slope, as a result of warding off the slope by no means appears to have been the precedence. However on one level Etienne Montero, the previous head of the European Institute of Bioethics, was right: When autonomy is entrenched because the guideline, exclusions and safeguards finally start to appear arbitrary and even merciless. That is the stress inherent within the euthanasia debate, the rationale why the follow, as soon as set in movement, turns into exceedingly tough to restrain. As Canada’s former Liberal Senate chief James Cowan as soon as put it: “How can we flip away and ignore the pleas of struggling Canadians?”
Ultimately, essentially the most significant guardrails on MAID might effectively develop into the suppliers themselves. Legislative will has usually been fastened within the path of extra; public opinion sparkles in response to particular points, however to this point stays largely settled. If MAID reaches a restrict in Canada, it’ll occur solely when practitioners determine what they will tolerate—morally or, in a system with a shrinking provide of suppliers, logistically. “You can’t ask us to supply on the fee we’re offering proper now,” Claude Rivard, who has determined to not settle for advance requests, advised me. “The restrict will at all times be the analysis and the supplier. It’ll relaxation with them. They must do the analysis, they usually must say, ‘No, it’s not acceptable.’”
Lori Verigin, a nurse practitioner who supplies euthanasia in rural British Columbia, understands that individuals are involved about their “rights”—about “not being heard.” But she is the individual on the road relating to making certain these rights. That is what is usually misplaced in Canada’s dialog about assisted dying—concerning the push for growth within the educational papers or within the rarefied halls of Parliament. It isn’t the lawmaker or lawyer or pundit who should administer an injection and cease a coronary heart.
On a Thursday morning in June, I joined Verigin in her white Volkswagen as she drove to a MAID appointment close to the city of Path. I had not come to witness the supply, to be a stranger within the room. I used to be with Verigin as a result of I needed to grasp the before-and-after of MAID, the medical and emotional labor concerned in serving to somebody die. After eight years, Verigin had developed a well-recognized set of rhythms. She had her most popular pharmacy, the Customers Drug Mart near her residence, in Castlegar. This morning she had arrived because the doorways opened, prescription in hand; the pharmacist greeted her by identify earlier than putting on the counter a medium-size case resembling a sort out field. Verigin unsnapped the lid and confirmed that every thing was in place: the vials of midazolam, lidocaine, propofol, and rocuronium.
Verigin had recognized the affected person she was about to go to for a while, she advised me. Roughly a 12 months in the past, the affected person, affected by metastatic most cancers, had first requested about MAID; two weeks earlier, the affected person had checked out her and stated: “I’m simply achieved.” Verigin sipped from a to-go cup of espresso, decaf, as she drove. “I strive to not have an excessive amount of caffeine earlier than,” she stated.
En path to the affected person’s residence, we stopped by the hospital to select up Beth, an oncology nurse who usually assists Verigin. Beth has a present for assessing the vitality of the room, Verigin advised me, figuring out when somebody instantly wanted a hand-held or a Kleenex, thus permitting Verigin to completely concentrate on the injections. Beth’s mom, Ruth, had additionally helped resolve an issue Verigin had skilled early in her MAID follow—how obtrusive it felt rolling a clattering tray of syringes into the already fragile ambiance of a affected person’s residence. A quilter, Ruth had designed a smooth pouch with syringe inserts that rolled up like a towel. The material was tie-dyed and the smooth bundle was secured with a Velcro strap.

Jennilee Marigomen for The Atlantic
The home made roll-up pouch that Lori Verigin makes use of for MAID provisions
We parked exterior the affected person’s ranch-style residence, the white solar evident in a transparent sky. At precisely 10 a.m., the 2 clinicians walked to the door, the place moments later they had been greeted by one of many affected person’s grown kids. The door clicked faintly behind them.
I remained within the automotive, and for the following whereas watched the sluggish flip of different Thursdays: the neighbors throughout the road chatting of their sunroom, a canine lazing in entrance of a field fan. Then, at 11:39 a.m., a textual content message from Verigin: “We’re achieved.”
The clinicians had been quiet as they slid into the automotive. “Issues weren’t as predictable at the moment,” Verigin stated lastly. Discovering a vein had been unusually exhausting, they usually nervous momentarily that they won’t succeed, at one level leaving the room to debate their choices. “It’s at all times been a problem,” the affected person had reassured Beth. “You’re very mild. It’s not hurting.” The affected person had remained calm, unfazed. “I’m positive they had been doing that for the children, to be trustworthy,” Beth stated. “And possibly me too.”
As soon as the IV was in place, the supply had unfolded as deliberate: midazolam, lidocaine, propofol, rocuronium, loss of life. Afterward, the household had thanked and hugged the clinicians. “I believe the top consequence was good,” Verigin stated. “I in all probability could be feeling completely different if we couldn’t fulfill the affected person’s want, as a result of it’s additionally that huge buildup and the anticipation.”
Verigin described a guidelines of follow-up duties, together with the paperwork that must be submitted inside 72 hours. However for the remainder of the day, her duties as a nurse practitioner would take precedence. Solely later that evening, she stated, would she lastly have the house to replicate on the occasions of the morning. When the syringes and vials have been packed up, and the goodbyes to the survivors have been stated, it’s Lori Verigin who sits in her backyard alone. “We’re not simply robots on the market—we’re human beings,” she stated. “And there must be some respect and acknowledgment for that.” Verigin advised me she by no means needs to really feel “comfy” offering help in dying. The day she did, she stated, could be the day she knew to step again.

Jennilee Marigomen for The Atlantic
Lori Verigin in British Columbia
For Verigin, offering MAID to Observe 1 sufferers and even to some Observe 2 sufferers has “felt wise.” She defined: “Sure, I could also be nervous. Sure, I could also be unhappy. Sure, I’ll have plenty of, you understand, feelings round it, however I really feel prefer it’s the appropriate factor.” However relating to minors, or sufferers solely with psychological problems, or sufferers making advance requests, “I don’t know if I’ll really feel that approach.”
After dropping Beth off on the hospital in Path, Verigin headed to the Customers Drug Mart in Castlegar to return the sort out field. Verigin advised the pharmacist she could be again on June 18—the date of her subsequent provision. The pharmacist was grateful for the discover. She would go forward and order the propofol.
This text seems within the September 2025 print version with the headline “Canada Is Killing Itself.”



