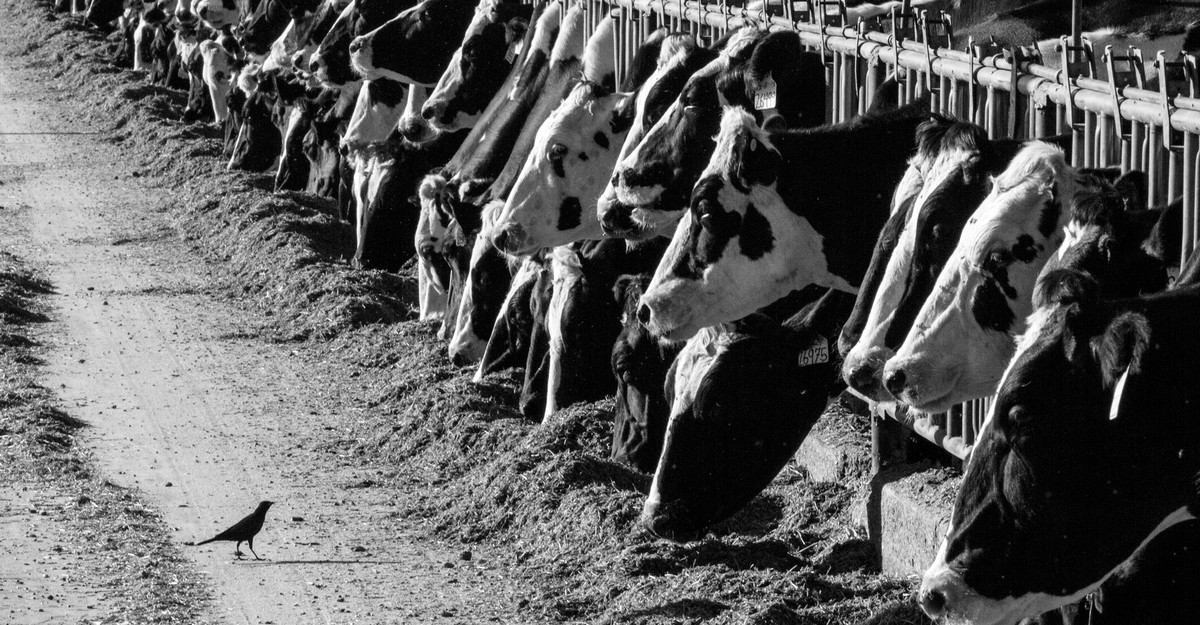
Three years in the past, when it was trickling into america, the bird-flu virus that just lately killed a person in Louisiana was, to most Individuals, an obscure and distant menace. Now it has unfold by way of all 50 states, affecting greater than 100 million birds, most of them home poultry; practically 1,000 herds of dairy cattle have been confirmed to be harboring the virus too. A minimum of 66 Individuals, most of them working in shut contact with cows, have fallen sick. A full-blown H5N1 pandemic will not be assured—the CDC judges the chance of 1 growing to be “reasonable.” However this virus is basically harder to handle than even a couple of months in the past and is now poised to turn out to be a persistent hazard to folks.
That didn’t should be the truth for america. “The experiment of whether or not H5 can ever achieve success in human populations is going on earlier than our eyes,” Seema Lakdawala, a flu virologist at Emory College, informed me. “And we’re doing nothing to cease it.” The story of chook flu on this nation may have been shorter. It may have concerned far fewer cows. The U.S. has simply chosen to not write it that approach.
The USDA and the CDC have doggedly defended their response to H5N1, arguing that their interventions have been appropriately aggressive and well timed. And governments, in fact, don’t have full management over outbreaks. However in contrast not less than with the infectious menace most distinguished in very latest reminiscence, H5N1 ought to have been a manageable foe, specialists exterior of federal companies informed me. When SARS-CoV-2, the virus that sparked the coronavirus pandemic, first spilled into people, virtually nothing stood in its approach. It was a brand-new pathogen, getting into a inhabitants with no preexisting immunity, public consciousness, exams, antivirals, or vaccines to struggle it.
H5N1, in the meantime, is a flu virus that scientists have been finding out because the Nineties, when it was first detected in Chinese language fowl. It has spent a long time triggering sporadic outbreaks in folks. Researchers have tracked its actions within the wild and studied it within the lab; governments have stockpiled vaccines towards it and have efficient antivirals prepared. And though this virus has proved itself able to infiltrating us, and has continued to evolve, “this virus remains to be very a lot a chook virus,” Richard Webby, the director of the World Well being Group Collaborating Centre for Research on the Ecology of Influenza in Animals and Birds, informed me. It doesn’t but appear able to transferring effectively between folks, and should by no means develop the flexibility to. Most human circumstances in america have been linked to a transparent animal supply, and haven’t turned extreme.
The U.S., in different phrases, might need routed the virus early on. As a substitute, companies tasked with responding to outbreaks and upholding animal and human well being held again on mitigation ways—testing, surveillance, protecting gear, quarantines of doubtless contaminated animals—from the very begin. “We’re underutilizing the instruments obtainable to us,” Carol Cardona, an avian-influenza knowledgeable on the College of Minnesota, informed me. Because the virus ripped by way of wild-animal populations, devastated the nation’s poultry, spilled into livestock, began infecting farmworkers, and amassed mutations that signaled higher adaptation to mammals, the nation largely sat again and watched.
Once I requested specialists if the outbreak had a transparent inflection level—a second at which it was essential for U.S. leaders to extra concertedly intervene—practically all of them pointed to the late winter or early spring of final 12 months, when farmers and researchers first confirmed that H5N1 had breached the nation’s cattle, within the Texas panhandle. This marked a tipping level. The soar into cattle, probably from wild birds, is assumed to have occurred solely as soon as. It might have been not possible to stop. However as soon as a pathogen is in home animals, Lakdawala informed me, “we as people have a variety of management.” Officers may have instantly halted cow transport, and arranged a cautious and concerted cull of contaminated herds. Maybe the virus “would by no means have unfold previous Texas” and neighboring areas, Lakdawala informed me. Dozens of people won’t have been contaminated.
These types of interventions would have not less than purchased extra of the nation time to provision farmworkers with info and safety, and maybe develop a plan to strategically deploy vaccines. Authorities officers may even have bought animals from the non-public sector to review how the virus was spreading, Cardona informed me. “We may have figured it out,” she mentioned. “By April, by Could, we might have identified how you can management it.” This sliver of alternative was slender however clear, Sam Scarpino, an infectious-disease modeler and flu researcher at Northeastern College, whose workforce has been carefully monitoring a timeline of the American outbreak, informed me. In hindsight, “realistically, that was most likely our window,” he mentioned. “We had been simply too sluggish.”
The virus, against this, picked up velocity. By April, a human case had been recognized in Texas; by the top of June, H5N1 had contaminated herds in not less than a dozen states and greater than 100 dairy farms. Now, lower than 10 months after the USDA first introduced the dairy outbreak, the variety of herds affected is verging on 1,000—and people are simply those that officers learn about.
The USDA has repeatedly disputed that its response has been insufficient, stating to The Atlantic and different publications that it shortly initiated research this previous spring to observe the virus’s actions by way of dairy herds. “It’s patently false, and a major discredit to the numerous scientists concerned on this work, to say that USDA was sluggish to reply,” Eric Deeble, the USDA’s deputy undersecretary for advertising and marketing and regulatory applications, wrote in an e mail.
And the company’s job was not a straightforward one: Cows had by no means been a identified supply of H5N1, and dairy farmers had by no means needed to handle a illness like this. The very best mitigation ways had been additionally commercially formidable. Essentially the most environment friendly methods to exploit cows invariably ship a plume of milk droplets into the air—and sanitizing gear is cumbersome. Plus, “the dairy business has been constructed round motion” of herds, a surefire method to transfer infections round too, Cardona informed me. The dairy-worker inhabitants additionally consists of many undocumented employees who’ve little incentive to reveal their infections, particularly to authorities officers, or heed their recommendation. Firstly of the outbreak, particularly, “there was a dearth of belief,” Nirav Shah, the principal deputy director of the CDC, informed me. “You don’t treatment that in a single day.” At the same time as, from the CDC’s perspective, that state of affairs has improved, such attitudes have continued to impede efforts to deploy protecting gear on farms and catch infections, Shah acknowledged.
Final month, the USDA did announce a brand new plan to fight H5N1, which requires farms nationwide to adjust to requests for milk testing. However Lakdawala and others nonetheless criticized the technique as too little, too late. Though the USDA has known as for farms with contaminated herds to boost biosecurity, implementation is left as much as the states. And even now, testing of particular person cows is basically left as much as the discretion of farmers. That leaves too few animals examined, Lakdawala mentioned, and cloaks the virus’s true attain.
The USDA’s plan additionally goals to get rid of the virus from the nation’s dairy herds—a tall order, when nobody is aware of precisely what number of cattle have been affected and even how, precisely, the virus is transferring amongst its hosts. “How do you eliminate one thing like this that’s now so widespread?” Webby informed me. Eliminating the virus from cattle could not really be an possibility. The virus additionally exhibits no indicators of exiting chook populations—which have traditionally been answerable for the extra extreme circumstances of avian flu which have been detected amongst people, together with the deadly Louisiana case. With birds and cows each harboring the pathogen, “we’re actually combating a two-fronted battle,” Cardona informed me.
Many of the specialists I spoke with additionally expressed frustration that the CDC remains to be not providing farmworkers bird-flu-specific vaccines. Once I requested Shah about this coverage, he defended his company’s concentrate on protecting gear and antivirals, noting that employee security stays “high of thoughts.” Within the absence of constantly extreme illness and proof of person-to-person transmission, he informed me, “it’s removed from clear that vaccines are the proper software for the job.”
With flu season effectively beneath approach, getting farmworkers any flu vaccine is among the most important measures the nation has to restrict H5N1’s menace. The unfold of seasonal flu will solely complicate well being officers’ skill to detect new H5N1 infections. And every time chook flu infects an individual who’s already harboring a seasonal flu, the viruses can have the chance to swap genetic materials, doubtlessly rushing H5N1’s adaptation to us. Aubree Gordon, a flu epidemiologist on the College of Michigan, informed me that’s her greatest fear now. Already, Lakdawala worries that some human-to-human transmission could also be taking place; america simply hasn’t applied the infrastructure to know. If and when testing lastly confirms it, she informed me, “I’m not going to be shocked.”